Visual Art by Artani Paris | Pioneer in Luxury Brand Art since 2002
Retirement’s unlimited free time feels liberating initially—then surprisingly empty. Without work structure dictating your days, you drift: sleeping irregular hours, skipping meals, abandoning exercise, losing track of time. Days blur together indistinguishably. The freedom you anticipated becomes purposeless void. “What did I accomplish today?” yields uncomfortable silence. This isn’t uncommon—many retirees struggle replacing decades of work routine with meaningful daily structure. The solution isn’t recreating work’s rigid schedule but designing intentional routines providing purpose, health, and satisfaction without feeling restrictive. This guide helps you build balanced daily routines matching your needs, energy levels, and interests. You’ll learn why routines matter more in retirement than working years (structure prevents drift, maintains health, creates satisfaction), how to design morning rituals energizing your day, incorporate physical activity sustainably, balance productivity with leisure without guilt, maintain social connections preventing isolation, and adapt routines as needs change with age. Whether you’re newly retired feeling lost or years into retirement seeking better balance, these strategies create days you look forward to—productive yet relaxed, structured yet flexible, purposeful yet enjoyable. Retirement’s gift isn’t endless leisure—it’s freedom to design days reflecting your values and priorities rather than employer demands. Let’s build routines making retirement years your best years.
Why Routines Matter More Than Ever in Retirement
Work provided automatic structure—wake time, commute, meetings, deadlines, lunch breaks, end-of-day. Retirement removes this scaffolding. Many discover structure wasn’t constraint but foundation enabling everything else.
The Science of Routine and Well-Being: Research consistently shows routines benefit mental and physical health—effects amplify with age. Circadian rhythm regulation—consistent sleep/wake times strengthen circadian rhythms governing sleep quality, hormone production, metabolism, immune function. Irregular schedules disrupt these systems causing: poor sleep (falling asleep difficult, waking frequently), daytime fatigue, weakened immunity, digestive issues, mood problems. Seniors especially sensitive—circadian disruption contributes to cognitive decline. Reduced decision fatigue—every decision depletes mental energy. Routines eliminate hundreds of daily micro-decisions: “What should I do now?” “When should I eat?” “Should I exercise today?” Conservation of mental energy for meaningful decisions. Habit formation and maintenance—routines make healthy behaviors automatic. Exercise at same time daily becomes habit requiring little willpower. Irregular exercise requires constant motivation (quickly abandoned). Sense of purpose and accomplishment—completing routine tasks creates satisfaction. Crossing items off daily checklist provides tangible progress feeling. Without routines, days end with vague dissatisfaction: “I was busy but accomplished nothing.” Anxiety reduction—predictability reduces anxiety. Knowing what comes next feels secure. Too much unstructured time paradoxically increases anxiety—freedom becomes overwhelming.
Common Retirement Routine Pitfalls: Complete lack of structure—”I’ll do whatever I feel like each day!” sounds ideal but often results in: sleeping late inconsistently (10 AM some days, noon others), skipping breakfast or eating irregularly, aimless internet browsing for hours, forgetting to exercise, isolated days without leaving home, guilt about “wasting” retirement. Over-structuring—opposite extreme: rigid schedules mimicking work, back-to-back activities leaving no rest, guilt when deviating from schedule, exhaustion from constant obligations. Both extremes fail. Lack of purpose—routines must include meaningful activities. Watching TV 6 hours daily is routine but not fulfilling. Social isolation—routines focused entirely on solo activities lead to loneliness. Must include regular social interaction. Neglecting health basics—busy retired people skip exercise, eat poorly, defer medical appointments despite having time. Inability to adapt—health changes, seasons change, life circumstances shift. Routines must flex.
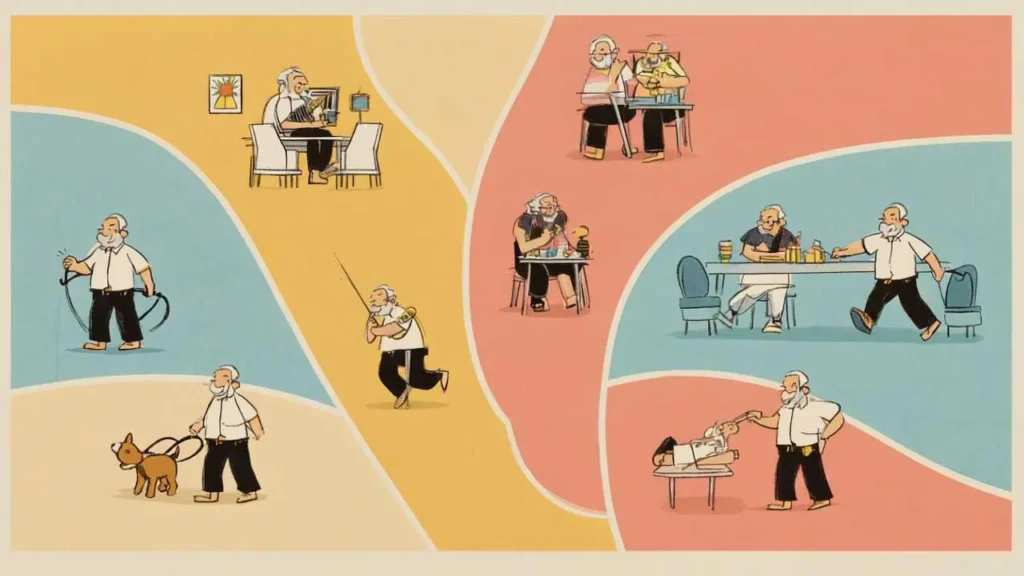
Components of Balanced Retirement Routine: Ideal routine includes these elements—not necessarily daily, but regularly throughout week. Physical activity—movement daily, formal exercise 3-5 times weekly. Maintains health, energy, independence. Mental stimulation—learning, reading, puzzles, hobbies. Prevents cognitive decline, provides satisfaction. Social connection—meaningful interaction with others. In-person ideal, phone/video acceptable. Prevents isolation depression. Productive activity—accomplishing something tangible. Gardening, volunteering, projects. Creates purpose. Leisure and relaxation—guilt-free enjoyment. Reading, hobbies, entertainment. Retirement should include pleasure. Self-care—sleep, nutrition, hygiene, medical appointments. Foundation enabling everything else. Spiritual/reflective time—meditation, prayer, journaling, nature walks. Whatever provides meaning and peace. Not everyone needs this but many benefit. Balance means all components present—not necessarily equal amounts daily but regularly throughout weeks.
Morning Routines: Starting Your Day With Purpose
How you start your day largely determines how the rest unfolds. Intentional morning routine sets positive tone, builds momentum, establishes control.
Establishing Consistent Wake Time: Why consistency matters—same wake time daily (within 30 minutes) strengthens circadian rhythm dramatically improving sleep quality. Even weekends—sleeping late Saturday disrupts rhythm causing “social jet lag.” Choosing your wake time—consider natural tendencies. Morning person? 6-7 AM ideal. Night owl? 7-8 AM. Compromise between natural preference and practical needs (appointments, activities). Most retirees thrive with 6:30-7:30 AM wake time—early enough to accomplish morning routine before late morning activities, late enough to avoid 5 AM alarm. Transitioning to earlier wake time—if currently waking 9-10 AM, shift gradually: Week 1: wake 8:30 AM, Week 2: wake 8:00 AM, Week 3: wake 7:30 AM, Week 4: wake 7:00 AM. Gradual 30-minute weekly shifts easier than sudden change. Waking naturally without alarm—goal for many retirees. Consistent sleep/wake times plus adequate sleep (7-8 hours) allows waking naturally. Initially use alarm as backup until pattern establishes. What if you’re not sleeping well? Poor sleep common in retirement (schedule irregularity, less physical activity, medical issues). Consistent wake time paradoxically improves sleep—trains body. Pair with good sleep hygiene: bedroom cool/dark, no screens 1 hour before bed, limit caffeine after 2 PM, regular exercise (not before bed).
Morning Movement and Exercise: Why morning exercise optimal—completed before other commitments interfere, boosts energy for entire day, improves focus and mood, establishes sense of accomplishment early, easier to maintain consistency (afternoon exercise often postponed). Types of morning movement—Gentle stretching (10-15 minutes)—upon waking, loosens stiff muscles and joints, improves flexibility gradually, can be done in bedroom before breakfast. Simple routine: neck rolls, shoulder shrugs, spinal twists, hamstring stretches, calf stretches. YouTube has numerous “morning stretching for seniors” videos. Walking (20-45 minutes)—most accessible exercise. Neighborhood walk, park, treadmill if weather poor. Brisk pace (can talk but slightly breathless). Alone for meditation or with spouse/friend for social connection. Observe neighborhood, listen to podcasts/audiobooks, or simply think. Yoga or tai chi (30-45 minutes)—improves flexibility, balance, strength, mindfulness. Many senior-specific classes (community centers, YouTube). Gentle pace appropriate for aging bodies. Swimming or water aerobics (30-45 minutes)—excellent low-impact exercise. Joint-friendly. Requires pool access. Home workout routine (20-30 minutes)—resistance bands, light dumbbells, bodyweight exercises. Focus on functional strength (ability to get off floor, carry groceries, climb stairs). Starting exercise habit—begin small: Week 1-2: 10-minute walk daily, Week 3-4: 15-minute walk daily, Week 5-6: 20-minute walk plus 10-minute stretching, Week 7+: 30-minute walk plus stretching, add strength training 2× weekly. Build gradually—overdoing causes injury and abandonment.
Breakfast and Morning Nutrition: Why breakfast matters—breaks overnight fast, stabilizes blood sugar (prevents mid-morning energy crashes), improves concentration, supports healthy weight (breakfast eaters less likely to overeat later), part of healthy routine rhythm. Skipping breakfast correlates with worse health outcomes in seniors. Components of healthy breakfast—Protein (20-30g)—eggs, Greek yogurt, cottage cheese, protein powder, nut butter, lean breakfast meat. Promotes satiety, preserves muscle mass (critical for seniors). Fiber (5-10g)—whole grain bread, oatmeal, berries, vegetables. Supports digestion, heart health, steady energy. Healthy fats—avocado, nuts, olive oil, fatty fish (smoked salmon). Supports brain health, satisfying. Limit sugar and refined carbs—sugary cereals, pastries, white bread cause blood sugar spikes and crashes. Quick healthy breakfast ideas—Greek yogurt with berries and granola (5 minutes), scrambled eggs with whole wheat toast and avocado (10 minutes), oatmeal with banana and walnuts (10 minutes), smoothie with protein powder, spinach, frozen fruit (5 minutes), whole grain toast with almond butter and sliced apple (5 minutes). Making breakfast routine sustainable—prep ingredients night before (cut fruit, measure oats), rotate 3-4 favorite meals (variety without decision fatigue), eat at consistent time (7:30-8:30 AM for most), sit down and eat mindfully (don’t eat standing or watching TV—creates eating routine).
Morning Planning and Intention Setting: Daily planning ritual (10-15 minutes)—after breakfast, before launching into day, review schedule and set intentions. What to do: Check calendar for appointments/commitments, identify 1-3 priorities for day (“Today I will: call doctor, work in garden 1 hour, read 2 chapters”), consider any obstacles or needs (errands, phone calls), visualize successful day. Benefits: Transforms vague day into purposeful day, prevents drift (“what should I do now?”), creates sense of control and direction, enables evening review (did I do what I intended?). Tools: Paper planner (many retirees prefer physical), digital calendar (Google Calendar, Apple Calendar), simple notebook (daily to-do list), habit tracking app (shows streaks, motivating). Avoiding over-planning: 1-3 priorities sufficient. Don’t create rigid hourly schedule (defeats retirement flexibility). Plan enough to provide direction, not so much to create stress. Some days priority is “rest and relax”—that’s valid.
| Time | Activity | Duration | Benefit |
|---|---|---|---|
| 6:30-7:00 AM | Wake, stretching, hygiene | 30 min | Consistent wake time, physical preparation |
| 7:00-7:30 AM | Exercise (walk, yoga, etc.) | 30 min | Physical health, energy boost, accomplishment |
| 7:30-8:00 AM | Shower, dress | 30 min | Self-care, readiness for day |
| 8:00-8:30 AM | Breakfast | 30 min | Nutrition, energy, routine |
| 8:30-8:45 AM | Daily planning, intention setting | 15 min | Purpose, direction, control |
| 8:45 AM | Day begins | – | Ready for productive, balanced day |
Structuring Your Days: Productivity and Leisure Balance
Mornings establish foundation—rest of day requires balance between accomplishment and enjoyment, structure and flexibility.
The “Anchor Activities” Approach: Rather than hourly schedule, identify 3-4 “anchor activities” occurring at consistent times providing structure without rigidity. Morning anchor—already covered: wake time, exercise, breakfast, planning. Midday anchor—lunch at consistent time (12:00-1:00 PM). Marks transition from morning productivity to afternoon. Includes: nutritious meal, brief rest or walk, social interaction (eat with spouse, call friend). Afternoon anchor—productive activity or hobby (2:00-4:00 PM). Gardening, volunteering, project work, errands. Something accomplished. Prevents entire afternoon vanishing into TV. Evening anchor—dinner time (6:00-7:00 PM), evening routine (discussed later). Anchors provide predictability. Between anchors, flexibility. Example day: 6:30 AM wake/exercise/breakfast (anchor), 9:00-11:30 AM flexible (reading, errands, appointments, hobbies), 12:30 PM lunch (anchor), 1:00-5:00 PM flexible (projects, social activities, rest, entertainment), 6:30 PM dinner (anchor), 7:30 PM+ evening routine (anchor). Structure without minute-by-minute control.
Productive Activities vs. Leisure: Both necessary—ratio depends on personality. Productive activities—provide accomplishment feeling, sense of purpose, tangible results. Examples: volunteering (food bank, library, hospital, mentoring), home projects (organizing, repairs, improvements, gardening), learning new skills (language, instrument, craft, technology), part-time work or consulting (income plus structure), creative pursuits (writing, painting, woodworking, photography), fitness goals (training for 5K, improving flexibility). How much productivity? 2-4 hours daily sufficient for most retirees. More exhausting, less enjoyable. Leisure activities—guilt-free enjoyment, relaxation, pleasure. Examples: reading (books, magazines, newspapers), entertainment (TV, movies, music, podcasts), hobbies (puzzles, games, crafts), social activities (coffee with friends, clubs, classes), nature (walks, birdwatching, gardening for pleasure), travel (day trips, exploration). How much leisure? 3-5 hours daily healthy. Entire days of leisure occasionally fine. Avoiding extremes—all productivity creates burnout (“retirement feels like second job”). All leisure creates emptiness (“I’m wasting my life”). Balance both based on energy and preferences. Some days productivity-heavy (major project), some days leisure-heavy (needed rest). Weekly balance matters more than daily.
Managing Energy Throughout the Day: Seniors often experience energy fluctuations—learning your patterns optimizes days. Common senior energy patterns—Morning larks—highest energy 7:00-11:00 AM, moderate 11:00 AM-3:00 PM, declining 3:00-6:00 PM, lowest evening. Strategy: productive activities morning, lighter activities afternoon, relax evening. Afternoon surge—moderate energy morning, dip late morning/early afternoon (post-lunch), surge 3:00-6:00 PM, decline evening. Strategy: light activities morning, nap or rest after lunch, productive activities mid-afternoon. Consistent energy—relatively steady throughout day (less common in seniors). Strategy: distribute activities evenly. Tracking your energy—for 1 week, note energy level each hour (1-10 scale). Patterns emerge. Schedule demanding activities during high-energy periods, rest/leisure during low-energy periods. Post-lunch dip—extremely common. 1:00-3:00 PM energy drops after lunch (natural circadian rhythm). Options: brief nap (20-30 minutes—longer causes grogginess), gentle walk (boosts energy), light reading or TV (accept lower energy period). Avoid scheduling demanding activities during this window. Respecting your energy—pushing through exhaustion counterproductive. Rest when needed. Consistent routine improves overall energy gradually.

Visual Art by Artani Paris
Social Connection and Community Engagement
Work provided automatic social interaction—coworkers, meetings, lunches. Retirement removes this, requiring intentional effort maintaining social connections critical for health and happiness.
Why Social Connection Is Non-Negotiable: Research overwhelmingly shows social isolation as dangerous as smoking 15 cigarettes daily. Physical health impacts—loneliness increases risk of: heart disease (29%), stroke (32%), dementia (50%), weakened immune system, higher blood pressure, inflammation. Isolated seniors die younger than socially connected peers. Mental health impacts—isolation causes or worsens: depression, anxiety, cognitive decline, poor sleep, decreased quality of life. Downward spiral: isolation leads to depression leads to more isolation. Loneliness vs. alone time—being alone isn’t problem (many enjoy solitude). Loneliness is feeling isolated, disconnected, unsupported—can occur even around people if connections shallow. Quality over quantity—one close friend better than ten acquaintances. Meaningful connections require: regular interaction (weekly minimum), genuine conversation beyond small talk, mutual support and care, shared activities or interests.
Building Social Connection Into Routine: Weekly commitments—join clubs/groups meeting regularly: book club (monthly discussions), exercise class (yoga, water aerobics, walking group 2-3× weekly), volunteer organization (weekly shifts at food bank, hospital, library), hobby groups (woodworking, quilting, photography, gardening), faith community (services, study groups, volunteering), senior center programs (classes, activities, meals). Benefit of scheduled activities: Automatic social interaction without planning each time, sense of belonging to community, shared purpose or interest, regular routine (Tuesdays 10 AM yoga becomes anchor). Maintaining existing friendships—schedule regular coffee/lunch with friends (weekly or biweekly standing date), phone calls with distant friends (same time weekly—Wednesdays call childhood friend), attend friend gatherings/celebrations (don’t decline due to inertia). Family connections—regular family dinners or video calls, involvement with grandchildren (babysitting, attending events), support to adult children (without overstepping). New friendships—retirement provides opportunity for new connections. Friends made through: classes, volunteering, neighbors (host block party, regular walks together), shared interests (meet at dog park, gym, library). Initiate: “Would you like to grab coffee sometime?” Most seniors receptive—also seeking connection.
Overcoming Social Barriers: Introversion—introverts need social connection too, just less frequently and in smaller groups. Strategy: one-on-one interactions rather than large groups, limited social activities (1-2 weekly instead of daily), balance with alone time for recharging. Mobility limitations—transportation challenges, physical difficulty attending events. Strategy: local activities within walking/easy driving, senior center programs often provide transportation, online groups/classes (Zoom book club, online courses), invite people to your home. Hearing loss—makes social situations frustrating, leads to withdrawal. Strategy: treat hearing loss (hearing aids dramatically improve socialization), smaller quiet venues rather than loud restaurants, inform friends about hearing challenges. Social anxiety—many seniors anxious about new social situations, especially after years in familiar work environment. Strategy: start with low-pressure situations (walking group—just walk together, class—shared focus, volunteer—task-oriented), bring spouse or friend initially, remember most seniors feel similarly, anxiety decreases with exposure. Geographic isolation—rural areas, moved away from friends/family. Strategy: prioritize building local connections even if takes time, use technology (video calls, online communities), consider relocation if isolation severe and alternatives exhausted.
Evening Routines: Winding Down and Reflection
Consistent Evening Routine Benefits: Evening routine as important as morning routine—signals day ending, prepares body for sleep, provides transition from activity to rest. Sleep preparation—consistent evening routine trains body to sleep. Same activities same time nightly tell brain “sleep coming soon.” Stress reduction—winding down process reduces cortisol (stress hormone) promoting relaxation. Reflection and gratitude—reviewing day increases satisfaction, recognizing accomplishments combats “I did nothing” feeling, gratitude practice improves mood and sleep quality. Connection with spouse/family—evening time for meaningful conversation, shared activities, reconnection after independent days.
Components of Healthy Evening Routine: Dinner at consistent time (6:00-7:00 PM)—earlier dinner allows digestion before bed (improves sleep), family meal (connection time), balanced nutrition (protein, vegetables, complex carbs, moderate portions). Light activity (6:30-7:30 PM)—evening walk (aids digestion, pleasant ritual), light gardening or hobby, household tasks (dishes, tidying). Avoid vigorous exercise (interferes with sleep). Leisure time (7:30-9:00 PM)—TV/movies, reading, conversation, games/puzzles, music, crafts. Enjoyable relaxation. Digital sunset (8:30-9:00 PM)—screens (TV, computer, phone) emit blue light suppressing melatonin (sleep hormone). Stop screens 1 hour before bed improves sleep. Alternatives: reading physical books, listening to music/audiobooks, conversation, journaling. Sleep preparation (9:00-9:30 PM)—light snack if hungry (warm milk, banana, small serving nuts—avoid heavy food), hygiene routine (brush teeth, wash face, medications), prepare bedroom (cool temperature 65-68°F, dark—blackout curtains or eye mask, quiet—white noise if needed), lay out tomorrow’s clothes (one less morning decision). Bedtime reflection (9:30-10:00 PM)—brief journaling (5 minutes): three things grateful for today, one thing accomplished, one thing learned. Ends day positively. Or meditation, prayer, reading inspirational/spiritual material. Consistent bedtime (10:00-10:30 PM)—same time nightly (within 30 minutes). With consistent wake time, creates 7-8 hour sleep window.
What If You Can’t Sleep? Sleep issues plague many retirees. Common causes—irregular sleep schedule (biggest factor), insufficient physical activity, daytime napping (over 30 minutes), worrying/rumination, medication side effects, sleep disorders (apnea, restless legs), underlying health conditions. Sleep hygiene basics—consistent sleep/wake times (most important), bedroom cool/dark/quiet, no screens 1 hour before bed, limit caffeine after 2 PM (6-hour half-life), limit alcohol (disrupts sleep quality), daily exercise (not near bedtime), expose to bright light daytime (strengthens circadian rhythm). If you can’t fall asleep—don’t lie awake frustrated. After 20 minutes, get up, do quiet activity (read, gentle stretching, meditation) until sleepy, return to bed. Repeat if necessary. Lying awake associates bed with wakefulness rather than sleep. If chronic insomnia—consult doctor. May need sleep study (diagnose apnea, restless legs), medication adjustment (some interfere with sleep), cognitive behavioral therapy for insomnia (CBT-I—highly effective, teaches techniques improving sleep). Don’t accept poor sleep as inevitable aging consequence—often treatable.
Adapting Routines as You Age
Flexibility Within Structure: Routines provide stability but must adapt. Seasonal adjustments—winter routines differ from summer. Winter: indoor exercise (gym, mall walking, YouTube workouts), earlier dinners (longer dark evenings), more indoor hobbies. Summer: outdoor activities (gardening, walks, patios), later dinners (enjoy daylight), travel. Adjust routines seasonally rather than fighting seasons. Health changes—surgery, illness, new limitations require temporary or permanent routine modifications. Post-surgery: gentler exercise, more rest periods, adapted activities. Chronic condition develops: accommodate limitations (seated exercises, delivery services for groceries, simpler cooking). Adjust routine to support health, not pretend limitations don’t exist. Energy changes with age—70-year-old routine may not work at 80. Generally: less intense exercise (switch running to walking, add rest days), shorter activity periods (2-hour projects become 1-hour), more frequent breaks, earlier bedtimes (many seniors shift earlier with age). Honor changing needs.
The “Good Enough” Principle: Perfectionism sabotages routines. Bad day? Simplified version still valuable. Full routine: 45-minute walk + strength training + yoga. Simplified: 15-minute walk. Simplified version infinitely better than nothing—and maintains routine momentum. Missing a day isn’t failure. Occasional missed workouts, skipped breakfast, irregular sleep inevitable. Resume next day without guilt. Routines are patterns, not perfect streaks. Progress over perfection. Inconsistent routine beats no routine. Flawed routine beats waiting for perfect routine. Start where you are, improve gradually. Self-compassion essential. Talk to yourself like supportive friend, not harsh critic. “I didn’t exercise today” not “I’m lazy and useless.” One day doesn’t define you.
Real Success Stories
Case Study 1: Ann Arbor, Michigan
David Martinez (67 years old, retired teacher)
David retired after 40 years teaching high school English. First 6 months felt wonderful—sleeping late, reading all day, no obligations. By month 7, depression crept in. Days blurred together indistinguishably. He’d wake 9:30 AM some days, noon others. Skip breakfast. Read or watch TV aimlessly. Realize at dinner he’d accomplished nothing. Feel guilty but repeat next day. Weight increased 15 pounds. Doctor visits skipped. Friends drifted (he’d decline invitations, too depressed). Wife concerned but unsure how to help. David described it: “I felt purposeless. Teaching gave my days structure and meaning. Retirement felt like falling into void.”
Turning point: Former colleague invited him to volunteer tutoring program at library—helping struggling readers. David agreed reluctantly. Required being there Tuesdays and Thursdays 10 AM-12 PM. To arrive on time, he needed wake 7:30 AM, exercise, shower, breakfast. Tutoring gave him purpose. He saw improvement in students. Felt valuable again.
This anchor prompted broader routine: Wake 7:30 AM daily (not just tutoring days—consistency better), 20-minute walk around neighborhood (gradual increase to 40 minutes), shower and dress properly (not staying in pajamas), 8:45 AM breakfast with wife (reconnection time), 9:30 AM-12:00 PM productive activity (tutoring, house projects, reading with purpose—book club meeting monthly), 12:30 PM lunch, 1:00-2:00 PM rest (read, light TV, nap if needed), 2:00-5:00 PM flexible (errands, hobbies, social activities, more projects), 6:00 PM dinner with wife, 7:00-9:00 PM leisure (TV, reading, games), 9:30 PM bedtime routine, 10:00 PM lights out.
Results after 6 months routine:
- Depression lifted completely—doctor reduced antidepressant dosage
- Lost 12 pounds—regular exercise plus eating at consistent times
- Sleep quality excellent—fell asleep quickly, woke refreshed
- Tutoring became highlight of week—purpose restored through helping students
- Joined book club (monthly meetings) and golf league (weekly games)—social connections strengthened
- Relationship with wife improved—more engaged, better mood, shared routines (morning walks together, evening conversation)
- Days feel satisfying—balance of productivity and leisure, accomplishment and rest
- Looks forward to retirement now—”I understand what people mean by ‘best years of your life’ now”
“The first six months of retirement nearly killed me emotionally. I went from highly structured teaching schedule to complete chaos. I thought freedom meant doing whatever whenever. Turns out freedom without structure is just emptiness. Creating daily routine saved my retirement. I wake up knowing what my day looks like—not minute-by-minute control, but enough structure to feel purposeful. Tuesday and Thursday tutoring sessions are anchors. Other days follow similar pattern even without tutoring. The routine isn’t restrictive—it’s liberating. I’m not wasting my retirement anymore. I’m living it fully.” – David Martinez
Case Study 2: Charleston, South Carolina
Barbara “Barb” and Kenneth “Ken” Anderson (71 and 73 years old)
The Andersons both retired same year—looked forward to unstructured days together. Reality disappointed. Ken became couch potato—TV morning to night. Barb felt lonely despite Ken’s constant presence (he wasn’t really “there”). They bickered frequently about nothing. Both gained weight. House chores neglected. Social life evaporated—used to socialize with work colleagues. Marriage strained—”We realized we didn’t know how to be together without work providing our individual identities and schedules,” Barb explained.
Crisis moment: Ken’s annual physical revealed pre-diabetes and high blood pressure. Doctor warned: “Your current lifestyle is killing you.” Simultaneously, Barb admitted marriage counselor she felt more lonely retired than when working—despite being with Ken constantly. Counselor suggested: individual routines within shared structure. Stop trying to do everything together. Maintain independence while sharing key moments.
They created new routine emphasizing: Independent mornings—both wake 7 AM but pursue individual activities. Ken walks alone 30 minutes (meditation time), Barb does yoga YouTube video 30 minutes. Gives space and individual health focus. Shared breakfast—8:15 AM together, catch up on morning activities, plan day. Connection point. Independent productive time—9:00 AM-12:00 PM each pursue own interests. Ken volunteers at Habitat for Humanity (woodworking background) 3× weekly, works in garage workshop other days. Barb volunteers at hospital 2× weekly, tends extensive garden, takes watercolor classes. Separate activities, separate fulfillment. Shared lunch—12:30 PM, brief reconnection. Flexible afternoon—sometimes together (errands, appointments, outings), sometimes apart (Ken golf league, Barb ladies’ book club). Varies daily. Shared dinner prep and meal—6:00 PM, cook together (teamwork, conversation), eat together (day review). Major connection point. Independent evening leisure—7:00-9:00 PM Ken watches sports, Barb reads or crafts. Same room but independent activities. Comfortable presence without forced interaction. Shared bedtime routine—9:30 PM prep, 10:00 PM bed.
Results after 1 year:
- Ken’s health transformed—lost 25 pounds, blood sugar normal range, blood pressure controlled, physically active through volunteering and golf, engaged and happy
- Barb’s loneliness resolved—individual social activities (hospital, book club, garden club), fulfillment from own interests, less resentful of Ken
- Marriage strengthened dramatically—time apart makes time together meaningful, conversation material from separate activities, reduced bickering (less constant togetherness), appreciate each other more, counselor discharged them (“You’ve figured it out”)
- House well-maintained—divided responsibilities, both more energetic
- Individual identities maintained—not just “the Andersons,” but individuals with own interests who happen to be married
- Friends increased—each has own social circle plus shared couple friends
- Both describe retirement as “finally what we hoped for”
“We almost ruined our marriage trying to do retirement ‘together.’ We thought being together all day would be romantic. It was suffocating. The routine saved us—specifically, building independence INTO our shared routine. Ken does his thing mornings, I do mine. We reconnect at breakfast. Then separate again. We’re together for meals and evenings, but we’re not joined at the hip. Sounds unromantic, but it’s actually brought us closer. We have things to talk about because we’re not experiencing every moment together. I’m happier individually, which makes me better company. Ken’s thriving with his woodworking and volunteering. We’re both living our best lives—separately and together.” – Barbara Anderson
Frequently Asked Questions
How do I create a routine without feeling like I’m back at work?
Key distinction: work routines were externally imposed and inflexible. Retirement routines should be self-designed and adaptable. Create routines providing structure without rigidity: use “anchor activities” at consistent times (wake, meals, exercise) rather than hourly schedules, leave flexibility between anchors—some days productive, some leisure-focused, include activities YOU want (not obligations), design around your energy patterns and preferences, allow deviations without guilt—routine is guide not prison. Think of routine as scaffolding supporting your chosen activities rather than cage restricting freedom. You’re in control—adjust anytime something isn’t working.
What if I’m a night owl and don’t want to wake up early?
Early wake time isn’t mandatory—consistency matters more than specific time. Night owls can create healthy routines waking 8-9 AM if that matches natural rhythm. However, consider: many activities (appointments, social events, volunteering) occur mornings, sleeping past 9 AM limits participation. Extreme night owl pattern (sleeping until noon, staying up past 2 AM) often indicates disrupted circadian rhythm benefiting from gradual adjustment. Compromise: wake 7:30-8:00 AM as middle ground. If naturally night owl with late bedtime (midnight), ensure 7-8 hour sleep (wake 7:30-8:30 AM). Consistent schedule still applies: same bedtime/wake time daily within 30 minutes strengthens circadian rhythm even for later times.
I feel guilty doing “nothing” even though I’m retired—how do I enjoy leisure without guilt?
Productivity guilt plagues many retirees—decades of work conditioning make leisure feel lazy. Reframe: Retirement isn’t endless vacation—it’s new life phase where YOU define productivity. Leisure IS productive if it: improves health (rest, hobbies reducing stress), maintains relationships (socializing, family time), provides joy and satisfaction (reading, gardening, entertainment). You earned this through decades of work. Combat guilt: schedule leisure like appointments (“2:00-4:00 PM reading time”—it’s planned activity, not laziness), balance productivity and leisure (2-3 hours productive activity daily satisfies achievement need, freeing remaining time for guilt-free leisure), recognize rest is necessary (bodies need recovery, especially aging bodies), remember nobody on deathbed regrets reading books, enjoying hobbies, relaxing. Guilt serves no purpose. Permission to enjoy leisure improves mental health.
What’s the ideal wake time for retirees?
No universal ideal—depends on individual circadian rhythm and lifestyle. General recommendations: 6:30-8:00 AM suits most retirees—early enough to participate in morning activities, late enough to allow adequate sleep (10:30 PM bedtime = 8 hours sleep), aligns with natural circadian rhythms (humans evolved as diurnal—daylight active). Waking before 6 AM unnecessary unless specific reason (early golf tee time, loved activity). Waking after 9 AM limits day structure, misses morning light exposure (critical for circadian health), may indicate too-late bedtime or poor sleep quality. Find YOUR ideal: experiment with different wake times for 1 week each, note energy levels, mood, productivity, sleep quality, choose time feeling best. Consistency matters more than exact time—7 AM daily better than varying 6-10 AM.
How do I maintain social connections if I’m naturally introverted?
Introverts need social connection too—just differently than extroverts. Strategies: choose quality over quantity—one close friend better than large friend group, one-on-one interactions instead of parties/large gatherings, select activities matching interests (book club, class, hobby group) providing natural conversation topics rather than forced small talk, limit frequency—1-2 social activities weekly sufficient for many introverts (extroverts need 4-5+), schedule alone time after socializing to recharge, recognize difference between introversion (energy from alone time) and social anxiety (fear of social situations)—latter may need therapy, social connection through shared activities (volunteering, classes) less draining than pure socializing, online communities provide connection without in-person energy drain (video calls, forums, email friends). Balance social needs with recharge needs—both legitimate.
What if my spouse and I have different routine preferences?
Common challenge—one morning person, one night owl. One active, one sedentary. One social, one introverted. Solutions: create individual routines within shared structure—separate mornings (each do own activities), shared meals (connection points), separate daytime activities (pursue individual interests), shared evening time, compromise on key routines (if one wakes 6 AM, other 8 AM, breakfast together 8:30 AM works for both), respect differences without judgment (neither wrong—just different), communicate needs clearly (“I need morning alone time” vs. silently resenting), divide household tasks by preference and energy (morning person makes breakfast, night owl handles evening tasks), maintain separate social circles plus shared friends (reduces resentment), schedule regular check-ins (“Is our routine working for you?”), adjust as needed. Anderson case study illustrates this well—independence within togetherness.
How much TV is too much in retirement?
No absolute number but guidelines exist. Research shows: 3+ hours daily associated with cognitive decline, sitting 6+ hours (TV common culprit) increases health risks significantly, passive entertainment (TV) less satisfying than active leisure (hobbies, socializing, reading). Healthy TV habits: limit to 2-3 hours daily maximum (some days less, occasional movie night more), break up viewing (not 4-hour marathon), combine with activity (stretch during show, stand/walk during commercials, use stationary bike/treadmill), choose quality programming (educational, meaningful) over mindless channel-surfing, social TV better than solo (watch with spouse, discuss shows, creates connection), balance with other leisure (reading, hobbies, socializing). Warning signs of excessive TV: using TV to avoid boredom without other interests, watching TV you don’t enjoy just to fill time, feeling guilty or depressed after watching, declining social invitations to watch TV, physical effects (weight gain, stiffness from sitting). TV isn’t evil but shouldn’t dominate retirement.
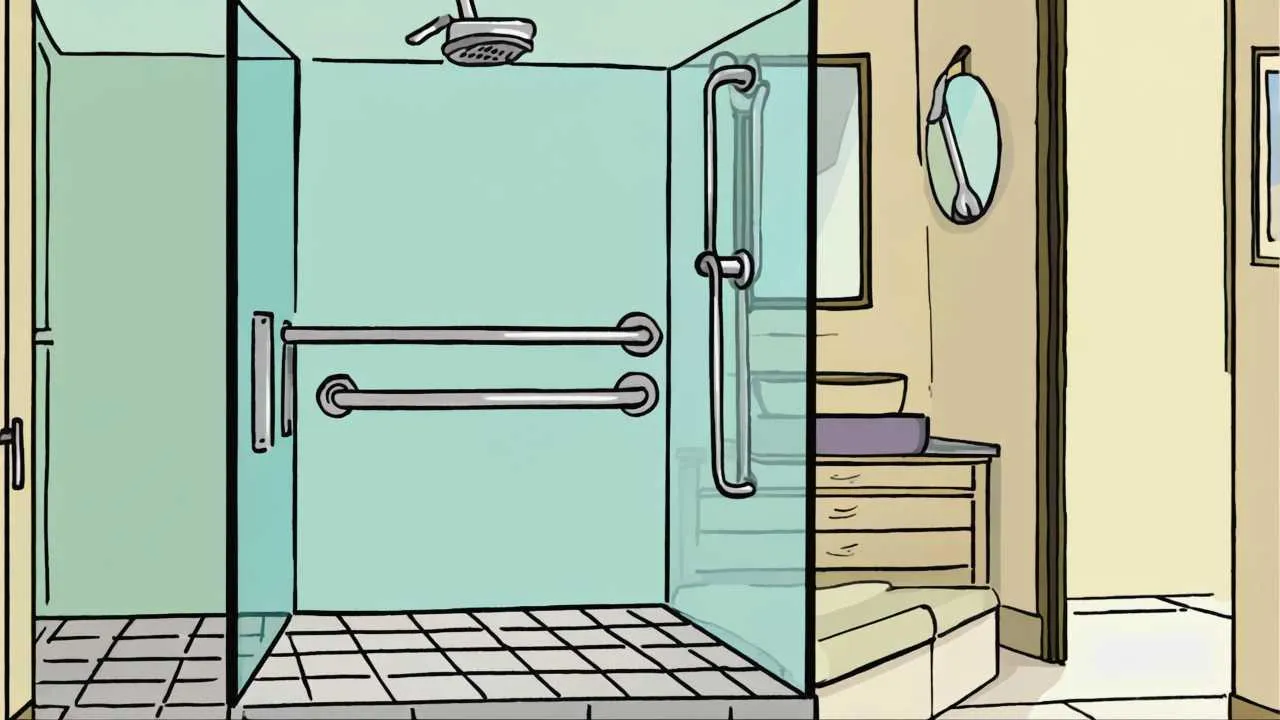
What if chronic pain or illness makes routine difficult?
Chronic conditions require routine adaptation not abandonment. Strategies: consult doctor about pain management improving function, adjust exercise (seated exercises, pool therapy, gentle yoga instead of impact activities), shorter activity periods with frequent breaks (30-minute tasks instead of 2-hour, rest between), flex routine—some days accommodate pain (high pain day = gentler routine), prioritize essential activities (medications, meals, basic hygiene) when pain severe, use “good days” productively (batch activities requiring more energy), build rest into routine (scheduled rest periods legitimize need), ask for help (grocery delivery, cleaning service, meal prep assistance), focus on what you CAN do rather than limitations, recognize routine maintaining health even if modified—consistency helps pain management. Example: arthritis prevents long walks—switch to pool walking 20 minutes 3× weekly. Routine exists, adapted to capabilities.
How long does it take to establish a new retirement routine?
Research on habit formation: simple habits (drinking water upon waking) take 18-21 days, complex behaviors (exercise routine) take 66 days average to become automatic, highly variable individual to individual (range: 18-254 days). Retirement routine recommendations: 3 months realistic expectation—first month awkward, lots of conscious effort, second month easier, habits forming, third month+ routine feels natural, requires less willpower. Tips for faster establishment: start with 2-3 core habits (wake time, exercise, meals) not entire routine simultaneously, use “implementation intentions” (specific plan: “I will walk at 7:30 AM in neighborhood for 30 minutes”), track habits (calendar X’s, app streaks—visual progress motivating), link new habits to existing ones (“after morning coffee, I will stretch for 10 minutes”), expect setbacks without abandoning—missing a few days doesn’t erase progress, be patient—worth the investment for decades of better retirement. Quick establishment: 1 month. Solid routine: 3 months. Automatic routine: 6 months.
Take Action: Building Your Retirement Routine
- Track your current patterns for 1 week before changing anything – Write down: daily wake time, meals (times and content), physical activity, productive activities, leisure activities, social interactions, bedtime. Note energy levels throughout day (1-10 scale). Identify patterns: when do you feel best? Worst? What activities energize vs. drain you? Current routine (even chaotic) provides starting point. Don’t judge—just observe and record honestly.
- Design your ideal morning routine on paper this week – Components to include: consistent wake time (choose based on natural tendency plus practical needs—7:00-8:00 AM for most), physical activity (start small—10-15 minutes, build gradually), breakfast (nutritious, consistent time), daily planning (10-15 minutes setting intentions). Write specific schedule: “7:00 AM wake, 7:15-7:30 AM stretch and walk, 7:45 AM shower/dress, 8:15 AM breakfast, 8:45 AM plan day.” Adjust times to your preferences. Morning routine is foundation—get this right, rest of day flows better.
- Implement morning routine for 3 weeks starting Monday – Begin with morning only—don’t overhaul entire life simultaneously. Commit to 3 weeks (habits start forming). Set phone alarms for each component initially. Expect resistance first week—normal. Week 2 gets easier. Week 3 feels more natural. Track daily (calendar X’s, journal, app). If you miss a day, resume next day without guilt. After 3 weeks, evaluate: what’s working? What needs adjustment? Modify as needed. Once morning routine feels automatic (6-8 weeks), add afternoon/evening components.
- Identify 2-3 weekly anchor activities providing social connection – Social connection non-negotiable for health—must be in routine. Options: volunteer commitment (weekly shifts—library, food bank, hospital, Habitat for Humanity), fitness class (yoga, water aerobics, walking group—schedule provides accountability), club or group (book club, hobby group, senior center programs), faith community (services, groups, volunteering). Choose activities you’ll enjoy (sustainability) and add to calendar as recurring appointments. Treat like doctor appointments—non-cancellable except for illness. Two weekly commitments minimum provides regular human interaction and routine structure.
- Schedule evening routine starting this week – Evening routine as important as morning for sleep quality and daily closure. Components: consistent dinner time (6:00-7:00 PM), light activity (walk, hobby, conversation), leisure time (reading, TV, games), digital sunset (screens off 1 hour before bed), sleep preparation (hygiene, medications, bedroom prep, brief reflection/journaling), consistent bedtime (within 30 minutes nightly). Write your schedule, follow for 2 weeks, assess sleep quality improvement. Adjust as needed. Pair with morning routine creates bookend structure for days.
- Review and adjust routine monthly for first 6 months – Last day of each month, evaluate: What’s working well? What feels forced or unenjoyable? Am I sleeping better? Do days feel purposeful? Am I maintaining social connections? Is health improving (exercise consistency, eating habits, weight, energy)? Do I feel satisfied end of day? Adjust based on honest assessment. Routine should serve you—not vice versa. Flexibility within structure. After 6 months, routine should feel natural requiring only seasonal adjustments or changes for major life events. Annual review sufficient thereafter.
Disclaimer
This article is provided for informational purposes only and does not constitute professional medical, psychological, or lifestyle advice. Health conditions, physical capabilities, and optimal routines vary by individual. Before starting any new exercise routine or making significant lifestyle changes, consult your physician, especially if you have chronic health conditions, mobility limitations, or are taking medications that might be affected by routine changes. Mental health concerns including depression or severe anxiety require professional evaluation and treatment beyond routine adjustments. The routines and schedules suggested are general guidelines requiring personalization to individual circumstances, preferences, and capabilities.
Information current as of October 2, 2025. Recommendations based on general health research and may not suit all individuals.
Related Articles
- Morning Routines Seniors in Their 60s Swear By for a Calm Day
- 2025 Senior Health: Start Your Day With AI Wellness Routines
Updated October 2025